Practice Policies & Patient Information
Access To Your Medical Records
A health record is any record of information relating to someone’s physical or mental health that has been made by (or on behalf of) a health professional. This could be anything from the notes made by a GP in your local surgery to results of an MRI scan or X-rays. Health records are extremely personal and sensitive.
They can be held electronically or as paper files and are kept by a range of different health professionals both in the NHS and the private sector. How can I access my records.
This is known as a subject access request.
You do not have to give a reason for applying for access to your health records. To save the NHS time and resources, it would be helpful if you would inform us – if you do not need access to your entire health record – of the periods and parts of your health records that you require, along with details which you may feel have relevance (e.g. consultant name, location, diagnosis etc.) You should also be aware that in certain circumstances your right to see some details in your health records may be limited in your own interest or for other reasons (e.g. to protect the privacy of third parties).
Please note:
- You can sign up for patient online services to your GP electronic record (please contact the practice for an application form).
- You can then look at your medical record whenever you want.
If you do wish to make a subject access request then:
- You can do this in writing (letter, email).
- You can make such a request verbally to a member of staff or a doctor or nurse that you are consulting with at the surgery.
Please let us know exactly what information you would like.
We will strive to provide the information within 28 calendar days.
There is usually no fee for this.
For more information, please visit www.ico.org.uk/your-data-matters.
Accessing someone else’s information
As a parent, family member or carer, you may be able to access services for someone else. We call this having proxy access. We can set this up for you if you are both registered with us.
To requests proxy access:
- fill in this admin request form
- collect a proxy access form from reception from 10am to 6pm
Linked profiles in your NHS account
Once proxy access is set up, you can access the other person’s profile in your NHS account, using the NHS App or website.
The NHS website has information about using linked profiles to access services for someone else.
Adult ADHD
This practice is not funded to provide comprehensive NHS services for adults with ADHD.
National guidance expects long-term involvement of specialists in reviewing these patients and their medical treatment, but this does not currently happen in Oxfordshire.
Therefore, the practice has taken the difficult decision that any new requests from specialists, both NHS and private, to prescribe ADHD medications to adult patients, will be declined.
We will also be making this clear to providers of ADHD services, at the point we refer patients for a diagnostic assessment. Care of adults already receiving ADHD treatments remains under careful review.
Patients may be able to access the care they need outside of the NHS, for instance by seeking a referral to a private provider from their NHS GP or NHS specialist.
As your NHS GP, we will not enter into “shared care” arrangements with private providers.
Patients should not be left without the care they need, due to a lack of comprehensive NHS funding, and our local representatives have raised this issue with local funding and decision-making groups. If you also wish to raise this issue, you may want to contact the “planned care team” at the local Integrated Care Board, bobicb.plannedcare@nhs.net , and/or your MP.
Chaperones
Patients are entitled to be accompanied by a chaperone for any consultation, examination or procedure.
If you would like one, please ask at Patient Services, mention it to your GP or contact us using our Contact the Practice form.
Commissioner’s details
Buckinghamshire, Oxfordshire, Berkshire West ICB
First Floor
Unipart House
Garsington Road
Cowley
OX4 2PG
Telephone: 01296 587220
General enquiries email: bobicb.enquiries@nhs.net
Confidentiality
All patients’ records are confidential. All our staff are trained in accordance with the Data Protection Act 2018 and work under strict rules of confidentiality.
Disability Access
All patient services are provided at ground floor level but if any assistance is required please ask at Patient Services and a member of staff will be happy to help.
Freedom of Information
The surgery has produced a publication in accordance with the Freedom of Information Act 2000.
If you have a request for any information in line with the Act please contact the practice manager using our Contact the Practice form.
GP Earnings
“All GP practices are required to declare the mean earnings (e.g.average pay) for GPs working to deliver NHS services to patients at each practice.”
The average pay for GPs who worked for six months or more in
Hightown Surgery in the last financial year was £47,730 before Tax and
National Insurance. This is for 9 part-time GP’s and 3 locum GP’s.
Named Accountable GP
All our patients now have a named, accountable GP, who will be responsible for the care and support that our surgery provides to them. We hope this will provide and continue to promote the continuity of care for our patients. If you’d like to know your named GP is please contact the surgery.
Your named GP will ensure that you receive the best possible level of care and support from our surgery and will work with other relevant healthcare professionals, who are involved in your care, to ensure that your care meets your individual needs.
Even though you have been assigned a GP, you can book appointments with any doctor or nurse at the practice.
Please contact us if you would like to change your named GP.
Non-NHS Work
The National Health Service provides most health care to most people free of charge, but there are exceptions. Some services provided are not covered under our contract with the NHS and therefore attract charges. GPs are not employed by the NHS, they are self-employed, and they have to cover their costs-staff, buildings, heating, lighting etc. – in the same way as any small business. The NHS pays the doctor for specific NHS work, but not for non NHS. The fee has to cover the doctors costs.
The fees charged are based on the British Medical Association (BMA) suggested scales and our Patient Services team will be happy to advise you about them along with appointment availability.
Examples where a patient can be charged include the following:
- Insurance claim forms
- Prescriptions for taking medication abroad
- Private sick notes
- Letters to third parties
- Vaccination certificates
- Certain travel vaccinations
- Private medical insurance reports
- Holiday cancellation forms
- Referral for private care form
- In certain instances fitness to work forms
Examples where another company can be charged include the following:
- Medical reports for an insurance company
- Some reports for DSS/Benefit agency
- Examinations for local authority employees
Where NHS and Private Care Meet
Patients are increasingly using private health providers. This is often a response to the increasingly long NHS waiting lists and these patients often feel that they are ‘helping’ the NHS by seeking private diagnosis and treatment. Unfortunately, many of these patients don’t realise that the interface between the NHS and private practice is complex.
Private providers may not be regulated in the same way as the NHS, and they may not follow NHS guidelines on diagnosis and management.
From the Thames Valley Commissioning Guidance:
- There is no obligation for the GP to prescribe treatment recommended by a private practitioner if it is contrary to local agreement or outside normal clinical practice.
- The NHS will not normally fund treatment recommended by a private practitioner if they are not usually commissioned in an area.
- Even if the patient can demonstrate they have benefited from private treatment this does not provide grounds for continuing the treatment on the NHS – clinical need should be assessed in the same way that we would assess an NHS patient in our area.
- Retrospective funding is not possible.
- There should be as clear as possible separation between NHS and private care.
- In one individual private consultation the patient must pay for all aspects within that consultation – any drugs prescribed or interventions.
- For ongoing care, the NHS GP can continue to prescribe if it would be normally provided on the NHS for that condition – we as GP’s are then taking on full responsibility for this. If the drug is not normally provided by primary care, we can enter into a ‘shared care agreement’ with ongoing monitoring by the private consultant if this is clearly set out and meant for GP shared care (for example gender services)
Frequently Asked Questions
What is covered by the NHS and what is not?
The government’s contract with GPs covers medical services to NHS patients. In recent years, more and more organisations have been involving doctors in a whole range of non medical work. Sometimes the only reason that GPs are asked is because they are in a position of trust in the community, or because an insurance company or employer wants to be sure that information provided is true and accurate
Why does it sometimes take my GP a long time to complete my form?
Time spent completing forms and preparing reports takes the GP away from the medical care of his/her patients. Most GPs have a very heavy workload – the majority of GPs work up to 60 hours a week and paperwork takes up an increasing amount of their time. In addition non-NHS work must be undertaken outside of NHS contracted time.
I only need the doctor’s signature – what is the problem?
When a doctor signs a certificate or completes a report, it is a condition of remaining on the Medical Register that they only sign what they know to be true. Therefore in order to complete even the simplest of forms, the doctor needs to check the patient’s entire record. Carelessness or an inaccurate report can have serious consequences for the doctor, with the General Medical Council or even the police.
Phone Call Recording Policy
Introduction
This policy outlines the practice’s call recording process.
The purpose of the call recording is to:
- Ensure practice staff act in compliance with procedures
- Ensure quality control
- Training, monitoring and service improvement
- Prevention of crime, misuse and protection of staff
Purpose
The purpose of this policy is to ensure that call recording is managed in line with the Data Protection Act 2018 and the NHS Records Management Code of Practice for Health and Social Care 2016 and data retention requirements. This will generally involve the recording of telephone conversations which is subject to the Telecommunications Act 1984.
The practice will make every reasonable effort to advise callers that their call may be recorded and for what purpose the recording will be used. This will normally be via a pre-recorded message within the telephone system and via the practice’s Privacy Notice. The voice file may be stored within the clinical system or within the telephone system to which the same rules of confidentiality will apply. They will be deleted after 3 years.
Where a patient requests to listen to a recording then this should be allowed with the general provision of data subject access under the Data Protection Act 2018.
Scope
This policy applies to all practice staff including contracted and temporary workers.
All calls via the telephone systems used in the practice will be recorded, including:
- All external incoming calls
- All external outgoing calls made by practice staff
- All internal incoming and outgoing calls made by the practice staff
- Call transfers
- Recording will automatically stop when the practice member terminates the call
Monitoring of Calls
Monitoring of call recordings will be undertaken by the Practice Manager or the Assistant Practice Manager. Any playback of recordings will take place in a private setting and where applicable, individuals should be given the opportunity to listen to the relevant recordings to receive feedback and developmental support.
All recordings and call recordings equipment will be stored securely encrypted, and access to these should be controlled and managed by the Practice Manager and the Assistant Practice Manager.
Access to the recordings is via the telephone system. This is a password protected portal accessed by the Practice Manager and the Assistant Practice Manager only.
Confidentiality
The Data Protection Act allows patients and staff access to information that is held about them and their personal data. This includes recorded telephone calls. Recordings should be stored in such a way that will enable easy access to the information relating to one or more individuals.
Requests for copies of telephone conversations can be made under the Data Protection Act as a ‘subject access request’. This can be in writing or verbal and after assessing whether the information can be released, the requestor can be invited to the practice premises to hear the recording.
If there is a request from an external body relating to the detection and prevention of crime (e.g. police) then requests for information should be directed to the Practice Manager.
Privacy Notice
Hightown Surgery
Privacy Notice
|
How we use your information
Your information, what you need to know.
This privacy notice explains why we collect information about you, how that information will be used, how we keep it safe and confidential and what your rights are in relation to this.
Why we collect information about you.
Health care professionals who provide you with care are required by law to maintain records about your health and any treatment or care you have received. These records help to provide you with the best possible healthcare and help us to protect your safety.
We collect and hold data for the purpose of providing healthcare services to our patients and running our organisation which includes monitoring the quality of care that we provide. In carrying out this role we may collect information about you which helps us respond to your queries or secure specialist services. We may keep your information in written form and/or in digital form.
Our Commitment to Data Privacy and Confidentiality Issues
As a GP practice, all of our GPs, staff and associated practitioners are committed to protecting your privacy and will only process data in accordance with the Data Protection Legislation. This includes the General Data Protection Regulation (EU) 2016/679 (GDPR) now known as the UK GDPR, the Data Protection Act (DPA) 2018, the Law Enforcement Directive (Directive (EU) 2016/680) (LED) and any applicable national Laws implementing them as amended from time to time. The legislation requires us to process personal data only if there is a legitimate basis for doing so and that any processing must be fair and lawful.
In addition, consideration will also be given to all applicable Law concerning privacy, confidentiality, the processing and sharing of personal data including the Human Rights Act 1998, the Health and Social Care Act 2012 as amended by the Health and Social Care (Safety and Quality) Act 2015, the common law duty of confidentiality and the Privacy and Electronic Communications (EC Directive) Regulations.
Details we collect about you.
Records which this GP Practice may hold about you will include the following:
- Personal Data – means any information relating to an identified or identifiable natural person (‘data subject’); an identifiable natural person is one who can be identified, directly or indirectly, in particular by reference to an identifier such as a name, an identification number, location data, an online identifier or to one or more factors specific to the physical, physiological, genetic, mental, economic, cultural or social identity of that natural person.
- Special Categories of Personal Data – this term describes personal data revealing racial or ethnic origin, political opinions, religious or philosophical beliefs, or trade union membership, and the processing of genetic data, biometric data for the purpose of uniquely identifying a natural person, data concerning health or data concerning a natural person’s sex life or sexual orientation.
- Confidential Patient Information – this term describes information or data relating to their health and other matters disclosed to another (e.g., patient to clinician) in circumstances where it is reasonable to expect that the information will be held in confidence. Including both information ‘given in confidence’ and ‘that which is owed a duty of confidence’. As described in the Confidentiality: NHS code of Practice: Department of Health guidance on confidentiality 2003.
- Pseudonymised – The process of distinguishing individuals in a dataset by using a unique identifier which does not reveal their ‘real world’ identity.
- Anonymised – Data in a form that does not identify individuals and where identification through its combination with other data is not likely to take place.
- Aggregated – Statistical data about several individuals that has been combined to show general trends or values without identifying individuals within the data.
How we use your information
Improvements in information technology are also making it possible for us to share data with other healthcare organisations for the purpose of providing you, your family, and your community with better care. For example, it is possible for healthcare professionals in other services to access your record with or without your permission when the practice is closed. Where your record is accessed without your permission it is necessary for them to have a legitimate basis in law. This is explained further in the Local Information Sharing at Appendix A.
Whenever you use a health or care service, such as attending Accident & Emergency or using Community Care services, important information about you is collected in a patient record for that service. Collecting this information helps to ensure you get the best possible care and treatment.
The information collected about you when you use these services can also be used and provided to other organisations for purposes beyond your individual care, for instance to help with:
- improving the quality and standards of care provided by the service.
- research into the development of new treatments and care pathways
- preventing illness and diseases
- monitoring safety
- planning services
- risk stratification
- Population Health Management
Safeguarding of children or vulnerable adults
If we have significant concerns or hear about an individual child or vulnerable adult being at risk of harm, we may share relevant information with other organisations, such as local authorities and the Police, involved in ensuring their safety.
Statutory disclosures
Sometimes we are duty bound by laws to disclose information to organisations such as the Care Quality Commission, the Driver and Vehicle Licencing Agency, the General Medical Council, Her Majesty’s Revenue and Customs and Counter Fraud services. In these circumstances we will always try to inform you before we are required to disclose, and we only disclose the minimum information that the law requires us to do so.
This may only take place when there is a clear legal basis to use this information. All these uses help to provide better health and care for you, your family and future generations. Confidential patient information about your health and care is only used like this were allowed by law or with consent.
Pseudonymised or anonymised data is generally used for research and planning so that you cannot be identified.
A full list of details including the legal basis, any Data Processor involvement and the purposes for processing information can be found in Appendix A.
How long do we hold information for?
All records held by the Practice will be kept for the duration specified by national guidance from Records Management Code of Practice – NHSX. Once information that we hold has been identified for destruction it will be disposed of in the most appropriate way for the type of information it is. Personal confidential and commercially confidential information will be disposed of by approved and secure confidential waste procedures. We keep a record of retention schedules within our information asset registers, in line with the Records Management Code of Practice for Health and Social Care 2021.
Individuals Rights under UK GDPR
Under UK GDPR 2016 the Law provides the following rights for individuals. The NHS upholds these rights in a number of ways.
- The right to be informed.
- The right of access
- The right to rectification
- The right to erasure (not an absolute right) only applies in certain circumstances.
- The right to restrict processing.
- The right to data portability
- The right to object
- Rights in relation to automated decision making and profiling.
Your right to opt out of data sharing and processing.
The NHS Constitution states, ‘You have a right to request that your personal and confidential information is not used beyond your own care and treatment and to have your objections considered’.
Type 1 Opt Out
This is an objection that prevents an individual’s personal confidential information from being shared outside of their general practice except when it is being used for the purposes of their individual direct care, or in particular circumstances required by law, such as a public health screening or an emergency like an outbreak of a pandemic disease. If patients wish to apply a Type 1 Opt Out to their record, they should make their wishes know to the Practice Manager.
National data opt-out (NDOO)
The national data opt-out was introduced on 25 May 2018, enabling patients to opt-out from the use of their data for research or planning purposes, in line with the recommendations of the National Data Guardian in her Review of Data Security, Consent and Opt-Outs.
The national data opt-out replaces the previous ‘type 2’ opt-out, which required NHS Digital not to use a patient’s confidential patient information for purposes beyond their individual care, for Planning or Research. Any patient that had a type 2 opt-out recorded on or before 11 October 2018 has had it automatically converted to a national data opt-out. Those aged 13 or over were sent a letter giving them more information and a leaflet explaining the national data opt-out. For more information go to National data opt out programme
To find out more or to register your choice to opt out, please visit www.nhs.uk/your-nhs-data-matters.
On this web page you will:
- See what is meant by confidential patient information.
- Find examples of when confidential patient information is used for individual care and examples of when it is used for purposes beyond individual care.
- Find out more about the benefits of sharing data.
- Understand more about who uses the data.
- Find out how your data is protected.
- Be able to access the system to view, set or change your opt-out setting.
- Find the contact telephone number if you want to know any more or to set/change your opt-out by phone.
- See the situations where the opt-out will not apply.
Right of Access to your information (Subject Access Request)
Under Data Protection Legislation everybody has the right of access to, or request a copy of, information we hold that can identify them, this includes medical records. There are some safeguards regarding what patients will have access to and they may find information has been redacted or removed for the following reasons.
- It may be deemed to risk causing harm to the patient or others.
- The information within the record may relate to third parties who are entitled to their confidentiality, or who have not given their permission for the information to be shared.
Patients do not need to give a reason to see their data. And requests can be made verbally or in writing. Although we may ask them to complete a form in order that we can ensure that they have the correct information required.
Where multiple copies of the same information is requested, the surgery may charge a reasonable fee for the additional copies.
Patients will need to provide proof of identity to receive this information. We will not share information relating to you with other individuals without your explicit instruction or without sight of a legal document.
Patients may also request to have online access to their data, they may do this via the NHS APP, or NHS Website.
Change of Detail
It is important that you tell the surgery if any of your contact details such as your name or address have changed, or if any of your other contacts details are incorrect including third party emergency contact details. It is important that we are made aware of any changes immediately in order that no information is shared in error.
Hightown Surgery administration online forms
Mobile telephone number
If you provide us with your mobile phone number, we will use this to send you text reminders about your appointments or other health screening information. Please let us know if you do not wish to receive text reminders on your mobile.
We also use the NHS Account Messaging Service provided by NHS England to send you messages relating to your health and care. You need to be an NHS App user to receive these messages. Further information about the service can be found at the privacy notice for the NHS App managed by NHS England.
Email address
Where you have provided us with your email address, with your consent we will use this to send you information relating to your health and the services we provide. If you do not wish to receive communications by email, please let us know.
Notification
Data Protection Legislation requires organisations to register a notification with the Information Commissioner to describe the purposes for which they process personal and sensitive information.
We are registered as a Data Controller and our registration can be viewed online in the public register at: http://ico.org.uk/what_we_cover/register_of_data_controllers
Any changes to this notice will be published on our website and in a prominent area at the Practice.
Data Protection Officer
Should you have any data protection questions or concerns, please contact our Data Protection Officer via the surgery at: bobicb-ox.hightown-admin@nhs.net
What is the right to know?
The Freedom of Information Act 2000 (FOIA) gives people a general right of access to information held by or on behalf of public authorities, promoting a culture of openness and accountability across the public sector. You can request any non-personal information that the GP Practice holds, that does not fall under an exemption. You may not ask for information that is covered by the Data Protection Legislation under FOIA. However, you can request this under a right of access request – see section above ‘Access to your information.’
Right to Complain
If you have concerns or are unhappy about any of our services, please contact the Practice Manager.
For independent advice about data protection, privacy, and data-sharing issues, you can contact:
The Information Commissioner
Wycliffe House
Water Lane
Wilmslow
Cheshire
SK9 5AF
Phone: 0303 123 1113 Website: https://ico.org.uk/global/contact-us
The NHS Constitution
The NHS Constitution establishes the principles and values of the NHS in England. It sets out the rights patients, the public and staff are entitled to. These rights cover how patients access health services, the quality of care you’ll receive, the treatments and programs available to you, confidentiality, information, and your right to complain if things go wrong.
https://www.gov.uk/government/publications/the-nhs-constitution-for-england
Reviews of and Changes to our Privacy Notice
We will keep our Privacy Notice under regular review. This notice was last reviewed in November 2023
Hightown Surgery
Privacy Notice – Appendix A
The Practice will share patient information with these organisations where there is a legal basis to do so.
| Activity | Rationale |
| Commissioning and contractual purposes
Planning
Quality and Performance
|
Purpose – Anonymous data is used by the Integrated Care Board (ICB) for planning, performance, and commissioning purposes, as directed in the practices contract, to provide services as a public authority.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Patients may opt out of having their personal confidential data used for Planning or research. Please contact your surgery to apply a Type 1 Opt out or logon to https://www.nhs.uk/your-nhs-data-matters/manage-your-choice/ to apply a National Data Opt Out
Processor – Buckinghamshire, Oxfordshire, and Berkshire West Integrated Care Board |
| Summary Care Record Including additional information | Purpose –The NHS in England uses a national electronic record called the Summary Care Record (SCR) to support patient care. It contains key information from your GP record. Your SCR provides authorised healthcare staff with faster, secure access to essential information about you in an emergency or when you need unplanned care, where such information would otherwise be unavailable.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’ Patients have the right to opt out of having their information shared with the SCR by completion of the form which can be downloaded here and returned to the practice. Please note that by opting out of having your information shared with the Summary Care Record could result in a delay to care that may be required in an emergency. Processor – NHS England |
| Research | Purpose – We may share anonymous patient information with research companies for the purpose of exploring new ways of providing healthcare and treatment for patients with certain conditions. This data will not be used for any other purpose.
Where personal confidential data is shared your consent will be required.
Where you have opted out of having your identifiable information shared for this Planning or Research your information will not be shared.
Legal Basis – · Articles 6(1)(a) and 9(1)(h) – explicit consent; or · Article 6(1)(c) (where we are legally obligated to share your personal data) for your standard personal data and Article 9(2)(j) (scientific research) for your health data.
Where identifiable data is required for research, patient consent will be needed, unless there is a legitimate reason under law to do so or there is support under the Health Service (Control of Patient Information Regulations) 2002 (‘section 251 support’) applying via the Confidentiality Advisory Group in England and Wales
Sharing of aggregated non identifiable data is permitted.
Processor – Clinical Practice Research Datalink |
| Individual Funding Requests | Purpose – We may need to process your personal information where we are required to fund specific treatment for you for a particular condition that is not already covered in our standard NHS contract.
The clinical professional who first identifies that you may need the treatment will explain to you the information that is needed to be collected and processed to assess your needs and commission your care; they will gain your explicit consent to share this. You have the right to withdraw your consent at any time, but this may affect the decision to provide individual funding.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Data processor – Buckinghamshire, Oxfordshire, and Berkshire West Integrated Care Board |
| Safeguarding Adults | Purpose – We will share personal confidential information with the safeguarding team where there is a need to assess and evaluate any safeguarding concerns and to protect the safety of individuals.
Consent is not required to share information for this purpose.
Legal Basis – Direct Care under UK GDPR:
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine
Data Processor – Hightown Surgery safeguarding lead |
| Safeguarding Children | Purpose – We will share children’s personal information where there is a need to assess and evaluate any safeguarding concerns and to protect the safety of children.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Consent may not be required to share this information.
Data Processor – Hightown Surgery safeguarding lead |
| Risk Stratification – Preventative Care | Purpose – ‘Risk stratification for case finding’ is a process for identifying and managing patients who have or may be at-risk of health conditions (such as diabetes) or who are most likely to need healthcare services (such as people with frailty). Risk stratification tools used in the NHS help determine a person’s risk of suffering a particular condition and enable us to focus on preventing ill health before it develops.
Information about you is collected from a number of sources including NHS Trusts, GP Federations, and your GP Practice. A risk score is then arrived at through an analysis of your de-identified information. This can help us identify and offer you additional services to improve your health.
If you do not wish information about you to be included in any risk stratification programmes, please let us know. We can add a code to your records that will stop your information from being used for this purpose. Please be aware that this may limit the ability of healthcare professionals to identify if you have or are at risk of developing certain serious health conditions.
Type of Data – Identifiable/Pseudonymised/Anonymised/Aggregate Data
Legal Basis
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processors – CSCSU |
| Public Health
Screening programmes (identifiable) Notifiable disease information (identifiable) Smoking cessation (anonymous) Sexual health (anonymous) Vaccination Programmes
|
Purpose – Personal identifiable and anonymous data is shared.
The NHS provides national screening programmes so that certain diseases can be detected at an early stage. These currently apply to bowel cancer, breast cancer, aortic aneurysms, and diabetic retinal screening service to name a few. The law allows us to share your contact information, and certain aspects of information relating to the screening with Public Health England so that you can be appropriately invited to the relevant screening programme. More information can be found at: https://www.gov.uk/topic/population-screeningprogrammes or speak to the practice.
Patients may not opt out of having their personal information shared for Public Health reasons. Patients may opt out of being screened at the time of receiving an invitation.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Data Processors – Oxfordshire Public Health |
| Direct Care
NHS Trusts Community Providers Pharmacies Enhanced care providers Nursing Homes Other Care Providers |
Purpose – Personal information is shared with other secondary care trusts and providers in order to provide you with individual direct care services. This could be hospitals or community providers for a range of services, including treatment, operations, physio, and community nursing, ambulance service.
Legal Basis – The processing of personal data in the delivery of direct care and for providers’ administrative purposes in this surgery and in support of direct care elsewhere is supported under the following:
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine
Processors – Oxford University Hospitals NHS Foundation Trust |
| Care Quality Commission | Purpose – The CQC is the regulator for the English Health and Social Care services to ensure that safe care is provided. They will inspect and produce reports back to the GP practice on a regular basis. The Law allows the CQC to access identifiable data.
More detail on how they ensure compliance with data protection law (including UK GDPR) and their privacy statement is available on our website: https://www.cqc.org.uk/about-us/our-policies/privacy-statement
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine
Processors – Care Quality Commission |
| Population Health Management | Purpose – Health and care services work together as ‘Integrated Care Systems’ (ICS) and are sharing data in order to:
• Understand the health and care needs of the care system’s population, including health inequalities. • Provide support to where it will have the most impact. • Identify early actions to keep people well, not only focusing on people in direct contact with services but looking to join up care across different partners.
Type of Data – Identifiable/Pseudonymised/Anonymised/Aggregate Data. NB only organisations that provide your care will see your identifiable data.
Anonymous data is also shared with the National Association of Primary Care to support work on health inequalities.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine
Data Processors – Optum, Cerner |
| Payments | Purpose – Contract holding GPs in the UK receive payments from their respective governments on a tiered basis. Most of the income is derived from baseline capitation payments made according to the number of patients registered with the practice on quarterly payment days. These amounts paid per patient per quarter varies according to the age, sex, and other demographic details for each patient. There are also graduated payments made according to the practice’s achievement of certain agreed national quality targets known as the Quality and Outcomes Framework (QOF), for instance the proportion of diabetic patients who have had an annual review. Practices can also receive payments for participating in agreed national or local enhanced services, for instance opening early in the morning or late at night or at the weekends. Practices can also receive payments for certain national initiatives such as immunisation programs and practices may also receive incomes relating to a variety of non-patient related elements such as premises. Finally, there are short term initiatives and projects that practices can take part in. Practices or GPs may also receive income for participating in the education of medical students, junior doctors, and GPs themselves as well as research. In order to make patient-based payments basic and relevant necessary data about you needs to be sent to the various payment services. The release of this data is required by English laws.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine
Data Processors – NHS England, ICB, Public Health |
| Patient Record data base | Purpose – Your medical record will be processed in order that a data base can be maintained, this is managed in a secure way and there are robust processes in place to ensure your medical record is kept accurate, and up to date. Your record will follow you as you change surgeries throughout your life.
Closed records will be archived by NHS England
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – EMIS and PCSE |
| Medical reports
Subject Access Requests
|
Purpose – Your medical record may be shared in order that:
Solicitors/persons acting on your behalf can conduct certain actions as instructed by you.
Insurance companies seeking a medical reports where you have applied for services offered by then can have a copy to your medical history for a specific purpose.
Legal Basis –
· Article 9(2)(a) – explicit consent for special-category data. We use a processor, iGPR Technologies Limited(“iGPR”), to assist us with responding to report requests relating to your patient data, such as subject access requests that you submit to us (or that someone acting on your behalf submits to us) and report requests that insurers submitted to us under the Access to Medical Records Act 1988 in relation to a life insurance policy that you hold or that you are applying for. iGPR manages the reporting process for us by reviewing and responding to requests in accordance with our instructions and all applicable laws, including UK data protection laws. The instructions we issue to iGPR include general instructions on responding to requests and specific instructions on issues that will require further consultation with the GP responsible for your care.
Processor – iGPR, Hightown Surgery, Solicitors, and insurance organisations |
| Medicines Optimisation
OptimiseRX
AnalyseRX
Oberoi
Medicines Management Team |
Purpose – your medical record is shared with the medicines management team pharmacists, in order that your medication can be kept up to date and any necessary changes to medication can be implemented.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – FDB, Virtual Pharmacist, Buckinghamshire, Oxfordshire, and Berkshire West Integrated Care Board |
| GP Federation
UCC
Evening and weekend GP Access Clinic,
NOxmed
GP Federation Service
Emergency Department
Minor Injury Unit
Out of Hours service
Urgent Care Centre
Primary Care Visiting Service
Hospital at Home Service
|
Purpose – Your medical record will be shared with the NOxmed in order that they can provide direct care services to the patient population. This could be in the form of video consultations, Minor injuries clinics, GP extended access clinics. The Federation will be acting on behalf of the GP practice.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – NOxmed, 111, OUH, OOH via Adastra IT system, PML, OXfed, |
| Primary Care Network
PCN |
Purpose – Your medical record will be shared with Banbury Alliance Primary Care Network in order that they can provide direct care services to the patient population.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – Hightown Surgery, Woodlands Surgery, Windrush Surgery |
| Smoking cessation | Purpose – personal information is shared in order for the smoking cessation service to be provided.
Only those patients who wish to be party to this service will have their data shared.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – Smoke Free Oxfordshire |
| Social Prescribers | Purpose – Access to medical records is provided to social prescribers to undertake a full service to patients dependent on their health social care needs.
Only those patients who wish to be party to this service will have their data shared.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – Age UK |
| Police | Purpose – Personal confidential information may be shared with the Police authority for certain purposes. The level of sharing and purpose for sharing may vary. Where there is a legal basis for this information to be shared consent will not always be required.
The Police will require the correct documentation in order to make a request. This could be but not limited to, DS 2, Court order, s137, the prevention and detection of a crime. Or where the information is necessary to protect a person or community.
Legal Basis – UK GDPR · Article 6(1)(c) – to comply with a legal obligation; and · Article 9(2)(j) – ‘for reasons of substantial public interest’
Processor – Police Constabulary |
| Coroner | Purpose – Personal health records or information relating to a deceased patient may be shared with the coroner.
Legal Basis – UK GDPR Article 6(1)(c) – to comply with a legal obligation and article 9(2)(h) health data.
Processor – The Coroner |
| Medical Examiner Service
(Change to community Medical Examiners Service – Oxfordshire) |
Purpose: Purpose: Medical records associated with deceased patients are outside scope of the UK GDPR. However, next of kin details are within the scope of the UK GDPR. We will share specified deceased patient records and next of kin details with the Medical Examiners within Oxfordshire University Hospitals NHS Foundation Trust.
Legal Basis: Article 6(1)(c) – necessary under a legal obligation to which the controller is subject”; and Article 9(2)(h)– “processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services”.
Processor: Medical Examiners service – Oxfordshire University Hospitals NHS Foundation Trust |
| Non-commissioned, private healthcare providers (e.g., BUPA, Virgin Care, etc.)
|
Purpose – Personal information shared with private health care providers in order to deliver direct care to patients at the patient’s request. Consent from the patient will be required to share data with Private Providers.
Legal Basis – Articles 6(1)(a) and 9(2)(a) Consented and under contract between the patient and the provider.
Provider – MIND, Healthshare, Primary Care Physio |
| Messaging Service
|
Purpose – Personal identifiable information shared with the messaging service in order that messages including appointment reminders; results; campaign messages related to specific patients health needs; and direct messages to patients, can be transferred to the patient in a safe way.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Provider – AccuRX – NHSAPP, Hightown Surgery website online communication system. |
| Remote consultation
Including –
Video Consultation
Clinical photography
Consult Connect (PhotoSAF) |
Purpose – Personal information including images may be processed, stored and with the patients consent shared, in order to provide the patient with urgent medical advice.
Patients may be videoed or asked to provide photographs with consent. There are restrictions on what the practice can accept photographs of. No photographs of the full face, no intimate areas, no pictures of patients who cannot consent to the process. No pictures of children
The Consultant Connect App allows clinicians to take IG compliant photos on their mobile phone. The photos are not saved on the phone but instead are emailed to the clinician’s NHS email address and saved in a secure cloud from where medical secretaries can access them for saving to records and attaching to local referral systems as appropriate.
Legal Basis – • Article 6(1)(e) ‘…necessary for the performance of a task carried out in the public interest or in the exercise of official authority…’; and • Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – AccuRX, Consultation Connect |
| MDT meetings | Purpose – For some long-term conditions, the practice participates in meetings with staff from other agencies involved in providing care, to help plan the best way to provide care to patients with these conditions. Personal data will be shared with other agencies in order that mutual care packages can be decided.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor – MS Teams |
General Practice Extraction Service (GPES)
|
Purpose – GP practices are required to provide data extraction of their patient’s personal confidential information for various purposes to NHS Digital. The objective of this data collection is on an ongoing basis to identify patients registered at General Practices who fit within a certain criterion, in order to monitor and either provide direct care, or prevent serious harm to those patients. Below is a list of the purposes for the data extraction, by using the link you can find out the detail behind each data extraction and how your information will be used to inform this essential work:
Legal Basis – All GP Practices in England are legally required to share data with NHS England for this purpose under section 259(1)(a) and (5) of the Health and Social Care Act 2012
Further detailed legal basis can be found in each link.
Any objections to this data collection should be made directly to NHS England. enquiries@nhsdigital.nhs.uk
Processor – NHS England
|
| Medication/Prescribing | Purpose: Prescriptions containing personal identifiable and health data will be shared with organisations who provide medicines management including chemists/pharmacies, in order to provide patients with essential medication regime management, medicines and or treatment as their health needs dictate. This process is achieved either by face-to-face contact with the patient or electronically. Pharmacists may be employed to review medication, Patients may be referred to pharmacists to assist with diagnosis and care for minor treatment, patients may have specified a nominated pharmacy they may wish their repeat or acute prescriptions to be ordered and sent directly to the pharmacy making a more efficient process. Arrangements can also be made with the pharmacy to deliver care and medication.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Patients will be required to nominate a preferred pharmacy.
Processor – Pharmacy of choice/Virtual Pharmacist |
| Professional Training | Purpose – We are a training surgery. Our clinical team are required to be exposed to on the job, clinical experience, as well as continual professional development. On occasion you may be asked if you are happy to be seen by one of our GP registrars, pharmacists, or other clinical team to assist with their training as a clinical professional. You may also be asked if you would be happy to have a consultation recorded for training purposes. These recordings will be shared and discussed with training GPs at the surgery, and also with moderators at the RCGP and HEE.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Recordings remain the control of the GP practice and they will delete all recordings from the secure site once they are no longer required.
Processor – RCGP, HEE, iConnect, Fourteen Fish |
| Telephony | Purpose – The practice use an internet-based telephony system that records telephone calls, for their own purpose and to assist with patient consultations. The telephone system has been commissioned to assist with the high volume and management of calls into the surgery, which in turn will enable a better service to patients.
Legal Basis – While there is a robust contract in place with the processor, the surgery has undertaken this service to assist with the direct care of patients in a more efficient way.
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Provider – Surgery Connect – X-ON |
| Learning Disability
Mortality Programme
LeDer |
Purpose: The Learning Disability Mortality Review (LeDeR) programme was commissioned by NHS England to investigate the death of patients with learning difficulties and Autism to assist with processes to improve the standard and quality of care for people living with a learning disability and Autism. Records of deceased patients who meet with this criteria will be shared with NHS England.
Legal Basis: It has approval from the Secretary of State under section 251 of the NHS Act 2006 to process patient identifiable information who fit within a certain criteria.
Processor : ICB, NHS England |
| Shared Care Record | Purpose: In order for the practice to have access to a shared record, the Integrated Care Service has commissioned a number of systems including GP connect, which is managed by NHS England, to enable a shared care record, which will assist in patient information to be used for a number of care related services. These may include Population Health Management, Direct Care, and analytics to assist with planning services for the use of the local health population.
Where data is used for secondary uses no personal identifiable data will be used.
Where personal confidential data is used for Research explicit consent will be required.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor: NHS England |
| Local shared care record | Purpose: Health and Social care services are developing shared systems to share data efficiently and quickly. It is important for anyone treating you to be able to access your shared record so that they have all the information they need to care for you. This will be during your routine appointments and in urgent situations such as going to A&E, calling 111 or going to an Out of hours appointment. It is also quicker for staff to access a shared record than to try to contact other staff by phone or email.
Only authorised staff can access the systems and the information they see is carefully checked so that it relates to their job. Systems do not share all your data, just data which services have agreed is necessary to include.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor: SCAS, UCC, PML, Hospital at Home |
| Anticoagulation Monitoring | Purpose: Personal Confidential data is shared with LumiraDX in order to provide an anticoagulation clinic to patients who are on anticoagulation medication. This will only affect patients who are within this criteria.
Legal Basis –
· Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine’
Processor : LumiraDX INRStar |
| ACR Project for patients with diabetes (and/or other conditions) | Purpose: Delivery of a programme, sponsored by NHS Digital, to monitor urine for indications of chronic kidney disease (CKD) which is recommended to be undertaken annually for patients at risk of chronic kidney disease e.g., patients living with diabetes. The programme enables patients to test their kidney function from home. We will share your contact details with Healthy.io to enable them to contact you and send you a test kit. This will help identify patients at risk of kidney disease and help us agree any early interventions that can be put in place for the benefit of your care. Healthy.io will only use your data for the purposes of delivering their service to you. If you do not wish to receive a home test kit from Healthy.io we will continue to manage your care within the Practice. Healthy.io are required to hold data we send them in line with retention periods outlined in the Records Management code of Practice for Health and Social Care. Further information about this is available at: https://lp.healthy.io/minuteful_info/.
Processor: NHS Digital, Healthy io |
| Child Health Information | Purpose: We wish to make sure that your child has the opportunity to have immunisations and health checks when they are due. We share information about childhood immunisations, the 6–8-week new baby check and breast-feeding status with health visitors and school nurses.
Legal Basis:
Processor: NHS Oxford Health Foundation Trust, NHS South Central and West Commissioning Support Unit, NHS England |
| Clinical audit | Purpose: To monitor the quality of the service provided to patients with long terms conditions and the safety of medicines. Some of this information may be held centrally and used for statistical purposes (e.g., the National Diabetes Audit or PRIMIS). When this happens, strict measures are taken to ensure that individual patients cannot be identified from the data.
Processor: Hightown Surgery, BOB-ICB |
| Invoice Validation | Purpose: Invoice validation is an important process. It involves using your NHS number to check which CCG is responsible for paying for your treatment.
Legal Basis: It has approval from the Secretary of State under section 251 of the NHS Act 2006 to process patient identifiable information who fit within a certain criterion.
Processor: Buckinghamshire, Oxfordshire, and Berkshire West Integrated Care Board. |
| National Fraud Initiative – Cabinet office | Purpose:
Legal Basis: statutory authority under Part 6 of the Local Audit and Accountability Act 2014. It does not require the consent of the individuals concerned under the Data Protection Act 1998. Data matching by the Cabinet Office is subject to a Code of Practice. For further information see:
Processor: Cabinet Office |
| National Registries | Purpose: National Registries (such as the Learning Disabilities Register)
Legal Basis: statutory permission under Section 251 of the NHS Act 2006, to collect and hold service user identifiable information without the need to seek informed consent from each individual service user.
Processor: Hightown Surgery |
| Supporting Locally Commissioned Services | Purpose: Integrated Care Boards support GP practices by auditing anonymised data to monitor locally commissioned services, measure prevalence and support data quality. The data does not include identifiable information and is used to support patient care and ensure providers are correctly paid for the services they provide.
Legal Basis: Article 6(1)e “processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller”
Article 9(2)h “processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services”. Processor: Buckinghamshire, Oxfordshire, and Berkshire West Integrated Care Board. |
| Suspected Cancer | Purpose: Data may be analysed in cases of suspected cancer by Nuffield Department of Primary Care Health Sciences, Oxford University to facilitate the prevention, early diagnosis, and management of illness. Measures are taken to ensure the data for analysis does not identify individual patients.
Legal Basis:
Processor: Nuffield Department of Primary Care Health Sciences, Oxford University. |
| Integrated Respiratory Team | Our practice is working with a team of specialists from a collaboration of the local health care trusts to provide enhanced care to patients who have certain established long term chest conditions, those who have recently had an emergency admission to hospital for a chest problem and those who have signs in their GP record that indicate that they may have undiagnosed lung disease. The team are working with us as honorary members of staff and will have access to relevant information in your electronic record. As well as offering face to face consultations to identified patients, they will be helping us to find patients who could benefit from additional clinical help. This service is a pilot project in 2019-2020, although it is hoped that it will become a long-term service when it is completed.
|
| NHS Community Pharmacist Consultation Service | Purpose: Patients contacting the practice with a minor illness can be offered a same day consultation with a pharmacist.
Legal Basis: patient consent
Processor: NHS England, NHS Digital, Sonar, PharmOutcomes |
| Hightown Surgery website | Purpose: Patients can complete online forms as a method of contacting the practice. The practice can also reply to patients and send information via this method.
Legal Basis: patient consent
Processor: Iatro |
| GP Connect | We use a facility called GP Connect to support your direct care. GP Connect makes patient information available to all appropriate clinicians when and where they need it, to support direct patients care, leading to improvements in both care and outcomes.
Authorised Clinicians such as GP’s, NHS 111 Clinicians, Care Home Nurses (if you are in a care home), Secondary Care Trusts, Social Care Clinicians are able to access the GP records of the patients they are treating via a secure NHS Digital service called GP connect. The NHS 111 service (and other services determined locally e.g. Other GP Practices in a Primary Care Network) will be able to book appointments for patients at GP practices and other local services.
Legal basis for sharing this data. In order for your Personal Data to be shared or processed, an appropriate “legal basis” needs to be in place and recorded. The legal basis for direct care via GP Connect is the same as the legal basis for the care you receive from your own GP, or another healthcare provider. · For the processing of personal data: Article 6.1 (e) of the UK GDPR: “processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller”. · For the processing of “Special Category Data” (which includes your medical information): Article 9.2 (h) of the UK GDPR: “processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services”.
Your rights Because the legal basis used for our care using GP Connect are the same as used in other direct care situations, the legal rights you have over this data under UK GDPR will also be the same. [NHS Digital] |
| ISAC
Integrated Severe Asthma Project |
Legal basis for sharing this data. In order for your Personal Data to be shared or processed, an appropriate “legal basis” needs to be in place and recorded. The legal basis for direct care via GP Connect is the same as the legal basis for the care you receive from your own GP, or another healthcare provider. · For the processing of personal data: Article 6.1 (e) of the UK GDPR: “processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller”. · For the processing of “Special Category Data” (which includes your medical information): Article 9.2 (h) of the UK GDPR: “processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services”. Processor: Hightown Surgery/OUH Pharmacy Team |
| Outcomes 4 Health/Pinnacle | Outcomes4Health is a web-based system which helps community clinicians provide services more effectively and makes it easier for commissioners to audit and manage these services. By collating information on clinical services, it allows local and national level analysis and reporting on the effectiveness of commissioned services, helping to improve the evidence base for community-based services. This system is used as part of our vaccination programme.
Legal basis for sharing this data. In order for your Personal Data to be shared or processed, an appropriate “legal basis” needs to be in place and recorded. The legal basis for direct care via GP Connect is the same as the legal basis for the care you receive from your own GP, or another healthcare provider. · For the processing of personal data: Article 6.1 (e) of the UK GDPR: “processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller”. · For the processing of “Special Category Data” (which includes your medical information): Article 9.2 (h) of the UK GDPR: “processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services”. Processor: Hightown Surgery/Outcomes4Health |
| Healthtech1 | Healthtech1 is a web-based system that integrates with the electronic health record to automation new patient registrations. It takes the information from the patient submitted online NHS England, PRF1 form and compares that information with the NHS Spine database. Mismatched data is flagged to the practice for checking, and correctly matched data is automatically processed into the EHR. The privacy policy of Healthtech1 can be found here.
Legal basis for sharing this data. In order for your Personal Data to be shared or processed, an appropriate “legal basis” needs to be in place and recorded. The legal basis for direct care via Healthtech1 is the same as the legal basis for the care you receive from your own GP, or another healthcare provider. · For the processing of personal data: Article 6.1 (e) of the UK GDPR: “processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller”. · For the processing of “Special Category Data” (which includes your medical information): Article 9.2 (h) of the UK GDPR: “processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services”.
Processor: Healthtech-1 Ltd. |
| City Sprint | From 1st October 2022 Primary Care Networks are required to provide Enhanced Access to services outside normal Monday to Friday working.
Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board (BOB ICB) have commissioned City Sprint to provide a secure blood transportation service to operate on Saturdays to collect samples from GP practices and transport to specimen laboratories. Patient data will be visible through partly transparent bags containing the sample bottles. Legal basis for sharing this data: NECESSARY FOR THE PERFORMANCE OF A TASK CARRIED OUT IN THE PUBLIC INTEREST OR UNDER OFFICIAL AUTHORITY VESTED IN THE CONTROLLER Processor: City Sprint Courier Services Ltd. |
We will keep our Privacy Notice under regular review. This notice was last reviewed on the 13th of December 2024.
Lawful basis for processing:
The processing of personal data in the delivery of direct care and for providers’ administrative purposes in this surgery and in support of direct care elsewhere is supported under the following Article 6 and 9 conditions of the UK GDPR:
- Article 6(1)(e) ‘…necessary for the performance of a task carried out in the public interest or in the exercise of official authority…’; and
- Article 9(2)(h) ‘necessary for the purposes of preventative or occupational medicine for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems and services…”
Requests from Secondary Care
Important information for patients attending an outpatient appointment (face to face, telephone, or video)
Please note that if the hospital decide you need a sick note, urgent prescription (needed within 7 days) or an onward referral it is THEIR RESPONSIBILITY and contractual obligation to organise it. It will ALWAYS be quicker for them to do this for you than for them to direct you back to us. Unfortunately, not everyone who works in the hospital knows this and we frequently have patients directed back to us in error by the hospital. This is making it more and more difficult for patients to get through to us on the phone or make appointments with us.
Please help us by making sure the hospital organises your sick note (for the whole time you will need to be off), urgent prescription or onward referral.
You can direct them to our website( Hightown Surgery ) or speak to PALS on 0800 328 7971 if you have any problems.
Thank you for helping us improve access to appointments for our patients.
The Hightown Partners
[Updated 23rd September 2024]
Suggestions, Comments and Complaints
We make every effort to give the best service possible to everyone who attends our practice.
However, we are aware that things can go wrong resulting in a patient feeling that they have a genuine cause for complaint. If this is so, we would wish for the matter to be settled as quickly, and as amicably, as possible.
To pursue a complaint, please complete our Complaints Form and we shall deal with your concerns appropriately. Further written information is available regarding the complaints procedure from Patient Services.
If something has gone well with your care at the surgery please let us know that too.
NHS Complaints Information
If you are not happy with the care or treatment you’ve received from an NHS service, you have the right to make a complaint.
To make a complaint you need to contact either:
- The NHS service that provided your care (e.g. GP practice, dentist or hospital) or;
- The commissioners of the service that provided your care. This will be either your local Clinical Commissioning Group or NHS England.
If you remain dissatisfied after you receive a full response, you can refer your complaint to the Parliamentary Health Service Ombudsman (PHSO). The PHSO is independent from the NHS and can undertake a review of the way in which your complaint has been managed.
If you need any support to make a complaint, or at any point during the complaints process, you can get free, confidential and independent advice from our local NHS complaints advocacy service.
For more information on the complaints procedure and your nearest NHS complaints advocacy service please visit www.nhs.uk or contact your local authority.
The Summary Care Record (SCR)
This is a national centralised database of limited medical information (allergies and medication only), extracted and uploaded from your GP record to NHS Digital. That information is then potentially available to medical staff nationwide.
In common with all GP surgeries, Hightown Surgery is required to extract and upload information from GP records to the national Summary Care Record (SCR) database, one of a number of NHS databases. Your Summary Care Record will contain all medication prescribed for you in the preceding 6 months, any repeat medication issued over the preceding 18 months, and any allergies or adverse reactions to medicines.
The information will potentially be available to healthcare professionals across England, for the purpose of your direct clinical care (a “primary” use of your information). The SCR is therefore a nationally available database. The information is extracted and uploaded to NHS Digital, who is therefore the data controller for the Summary Care Record database. There are no secondary uses of the SCR, and data uploaded to the SCR database is neither shared nor used beyond that required to provide direct medical care.
Who Can Access The Summary Care Record?
- Clinicians at SCAS NHS 111 Clinicians in Emergency Operations Centre
- Various departments at hospital
- Our community staff (district nurses, midwives and health visitors)
Community nurses have access to the GP records of our patients (through our EMIS Web clinical system).
If you do not wish to have, or continue to have, a Summary Care Record then you can opt-out at any time using our Summary Care Record Opt-out form. If you do opt-out, your uploaded data will be “blanked”, no one will be able to access it, and no further information about you will be uploaded from your GP record.
If you do opt-out, or if you have already opted out, then you can opt back in at any time and have a Summary Care Record created.
For more information, please visit www.digital.nhs.uk/summary-care-records-scr.
Training Practice
We have been a training practice since 1992. We enjoy and are committed to teaching and see the benefits it brings to patients, the practice, and the profession. We are proud of our successful training record and 3 of our current doctors actually started here as trainees.
We are part of the Banbury GP Vocational Training Scheme within the Oxford Deanery.
The whole practice participates in GP Training, and we also teach a variety of other health professionals; so far including community nurses, health visitor and midwifery students, student counsellor and a pharmacist. We also have Oxford medical students on short term attachments each autumn.
GPs in Training
Doctors who train with us are fully qualified and have selected general practice as their career speciality. They have completed at least 2 years in hospital posts, and some have prior GP experience too.
Postgraduate medical training has recently been modernised so that more doctors have the opportunity to learn in general practice, whatever their final career aspirations. This means we now have the opportunity to expand our teaching role, to include recently qualified doctors who wish to learn more about primary care. They join us for 4-6 months and have a greater level of supervision than our 1-year registrars (for simplicity we refer to them all as registrars).
GP Registrars in Practice
What do registrars do?
Registrars will:
- Sit and observe consultations
- Conduct joint consultations with their supervising GP
- Consult on their own, always with a backup GP
- Occasionally video record their consultations for personal teaching purposes
You may be told you are seeing a GP registrar when you make your appointment, and the doctor will also introduce themselves as a GP registrar when they greet you. You will always be asked if you are happy for a registrar or student to sit in on your consultation but if you are uncomfortable with this please decline.
As a training practice we will always seek your written permission if the registrar is videoing their consultations. Physical examinations will be off camera and you can ask for the camera to be switched off at any time during the consultation.
The videos are only viewed by the GP registrars and their supervising GP’s and are an invaluable tool for teaching consultation skills. Some videos can be used for the RCA examination, so may be viewed by an external examiner (which you will be asked separate permission for).
How does This Benefit Patients?
As a training practice we have to demonstrate and maintain the highest standards of healthcare for our patients, as well as providing an excellent learning environment for GP registrars. We are rigorously externally assessed every 3 years for excellence in organisational, clinical, and educational performance.
Registrars also increase the number of available appointments, bring fresh ideas and enthusiasm, and share the most up to date hospital practice with us.
We feel privileged to be involved in training the doctors of the future and hopefully encouraging them to aspire to be excellent GPs as defined by the Royal College of General Practitioners (RCGP).
Information for potential learners:
For any further information please contact Dr Kate Smith (trainer) or Mr Stanford Jeffery the practice manager.
Research
The practice has traditionally been involved with primary care research, in particular with Dr Lehman’s work on heart failure and Dr Hin’s on Coeliac Disease and on vitamin B12 deficiency. Dr Hin retired in July 2012 but continued to run a research project on vitamin D deficiency, details of which you may have seen in the surgery and many of you kindly participated in, this concluded in 2014.
We take part in projects run by reputable, outside agencies (often Oxford University or the Oxford Hospitals).
We have also been involved in the ATAFUTA trial for treatments for urinary tract infection and the COMBO trial for use of supportive IT systems for people with bipolar disorder.
It will always be made clear to you if any of your care is linked in any way to research. We are justifiably proud of the achievements so far in this area.
Zero Tolerance
Zero Tolerance Policy – Patient Behaviour
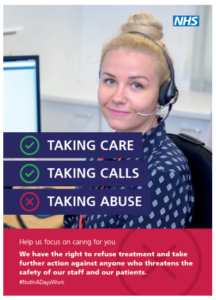
As an employer, Hightown Surgery has a duty of care for the health, safety and wellbeing of its staff. The practice also has a legal responsibility to provide a safe and secure working environment for staff. Staff mental health is as important as their physical health.
All patients and staff are expected to behave in an acceptable, respectful manner.
The practice follows the NHS guidance concerning Zero Tolerance.
Any incident in which an employee is abused, threatened or assaulted in circumstances relating to their work is unacceptable and not tolerated.
This includes the serious or persistent use of verbal abuse, aggressive tone and/or language and swearing/foul language.
Staff should not be left upset and distressed following an interaction with a patient.
All instances of actual physical abuse or threatening behaviour on any doctor or member of staff, by a patient or their relatives will be reported to the police as an assault.
We expect all patients to be responsible and avoid attending the surgery under the influence of alcohol or illegal drugs. Any alteration of prescriptions is illegal and will not be tolerated.
The General Medical Council States In Good Medical Practice that: “In rare circumstances, the trust between you (the Practice) and a patient may break down, and you may find it necessary to end the professional relationship. For example, this may occur if a patient has been violent to you or a colleague, has stolen from the premises, or has persistently acted inconsiderately or unreasonably.”
This includes unnecessarily persistent or unrealistic service demands that cause disruption. Examples of this include, but are not limited to :
- Demanding to only speak to a specific team member
- Refusing appointments with an appropriate clinician for the presenting care need i.e. insisting on a GP appointment when seeing a pharmacist or nurse prescriber is most appropriate or refusing to see an available GP for your presenting care need when your preferred GP is unavailable
- Refusing to access the service in the appropriate manner i.e. sending emails/texts instead of using the NHS Digital approved digital consultation service
- Demanding a same day appointment for a routine clinical need (after triage by trained staff) – this deprives access to urgent care services for those who genuinely need it
- Contacting individuals directly via social media or personal email instead of through the practice contact channels
The practice has a finite number of available appointments, and you may be directed to a clinician who is not a GP, or your preferred GP, but who is appropriately qualified to manage the presenting care need. We provide a named GP service, but we cannot always accommodate requests to speak to the same GP due to high patient demand for appointments.
If you are seriously unhappy with the quality of service you have the right to register with another practice without notifying us. Similarly, on the very rare occasions when a patient breaches this policy, we have the right to remove the patient from our Practice list.
Examples of Unacceptable Standards of Behaviour
In exceptional circumstances, a breakdown may occur between a doctor and their patient. If the breakdown is of a serious nature e.g. serious physical or verbal abuse to any member of the practice team, the doctors may feel that the doctor/patient relationship has been compromised. Steps may be taken to have the patient removed immediately from the practice list. Where possible, conciliation would always be the preferred route. Reasons for removal will be given in writing.
Where we deem an incident is not serious enough to warrant immediate removal, we will issue a first and final warning.
You will be removed from our patient list immediately when we have needed police assistance or have made a report to the police.
The following are examples of when you may be issued with a first and final warning or removed from our patient list dependent on the severity of the incident.
- Violence.
- Excessive noise e.g. recurrent loud or intrusive conversation or shouting.
- Threatening or abusive language involving swearing or offensive remarks.
- Racial or sexual remarks.
- Aggressive, forceful tone and/or language that upsets staff.
- Malicious allegations relating to members of staff, other patients or visitors.
- Offensive gestures or behaviours.
- Abusing alcohol or drugs on practice premises.
- Drug dealing on practice premises.
- Wilful damage to practice property.
- Threats or threatening behaviour.
- Theft.
- Persistent and/or unrealistic demands on the service
- Repeated derogatory comments about the practice or individuals either verbally, in writing/digitally or on social media platforms – this applies to factual and false information as we have a process to feedback dissatisfaction.
This list is not exhaustive and there may be other occasions where we have cause to issue a warning or remove you from our patient list. If you are unhappy with the practice we have a complaints procedure to assist you, or you have the choice to register with another practice – there really is no need for unpleasant behaviour with these options available to support you.
We trust this policy is clear and supports a mutually respectful environment for patients and staff.